
The SARS-CoV2 virus causes COVID-19
An RNA virus enters a cell and uses normal cellular processes to make copies of itself. SARS-CoV2 has this replication cycle. As SARS-CoV2 exits the cell by exocytosis it doesn’t damage the cell.
The corona virus SARS-CoV2 is the agent responsible for causing the COVID-19 respiratory disease. Viruses are small bundles of nucleic acids, covered by protein to protect them from environmental damage. If the virus is able to enter a proper host cell, this bundle has a set of instructions that allows the virus to use normal processes in the host cell to produce copies of itself. This virus was initially discovered and described in December, 2019 in China and the name COVID-19 is derived from “Corona Virus Disease 2019”. This is the replication cycle of a virus like SARS-CoV2 in a human cell:
When the world discovers a virus, scientific and health authorities obtain the following information: origin of virus, genomic sequence (genome), and transmission method, effectiveness of transmission, symptoms and disease progression. This strategy allows health systems to prepare the tools necessary to control infection in an individual, reduce the number of infections in the population, predict future epidemics and avoid pandemics.
The SARS-CoV2 is related to SARS-CoV1, responsible for the 2002-2003 SARS epidemic. There is no evidence this virus was developed as a biological weapon.
The SARS-CoV2 appears to be related to SARS-CoV1 that caused the 2002-2003 SARS epidemic, that was largely restricted to South East Asia (Gorbalenya et al., 2020). Both of these viruses are part of a large group of viruses that infect many mammals and in humans may cause respiratory diseases (such as the common cold). Corona viruses cause up to one third of all colds (Maier, Bickerton, & Britton, 2015). In the wild bats are the natural reservoirs for both SARS-CoV1 and SARS-CoV2 (Benvenuto et al., 2020).
COVID-19 is a zoonotic disease
Occasionally, a viruses have a small changes to their genetic sequence (mutation) which may alter its infectivity and allow it to infect humans. Housing bats and other wild animals close to humans causes transmission of a disease from an animal to a human, an event known as zoonosis and the disease is referred to as a zoonotic disease. Occasionally there is an intermediate animal that transmits disease to humans, such as a domesticated animal. This is the case for camels and the coronavirus responsible for the Middle Eastern Respiratory Syndrome. Domestic animals can’t transmit the SARS-CoV2 to humans. SARS-CoV2 can infect domestic cats and transmit to other cats. Therefore, cats should be considered reservoirs for the virus (Shi et al., 2020), although there is no evidence that cats can infect humans.
The SARS-CoV2, which causes COVID-19 is not transmitted from domestic animals to humans.
It is very rare that viruses evolved to infect another animal, such as bats or cows, infect humans. The virus has proteins on its surface that have evolved to infect specific species. Bats have tolerant immune systems which allow the virus to replicate inside their cells without causing the bat harm. The virus can remain in these bat populations for a long time (hundreds or thousands of years), acquiring mutations. Eventually, and through a random process, enough mutations accumulate to allow the virus to infect cells in another species of animal (Parrish et al., 2008). It is important to determine the source of the virus. This helps us understand how different the virus that infects humans is from its progenitor found in wild life. That information is useful in tracking disease and predicting future outbreaks.
genomic sequences yield important information
The rate at which viruses acquire mutations is important because it can tell us the origin of the virus (Benvenuto et al., 2020). Nextstrain.org has a weekly updated graph containing information that shows how small molecular changes allow us to track the spread of the virus. Knowing changes to the sequence allow scientists to develop drugs that inhibit infection or develop an effective vaccine. The following figure shows different parts of the viral “life-cycle” and therapeutic opportunities being explored (Smith, Bushek, & Prosser, 2020).
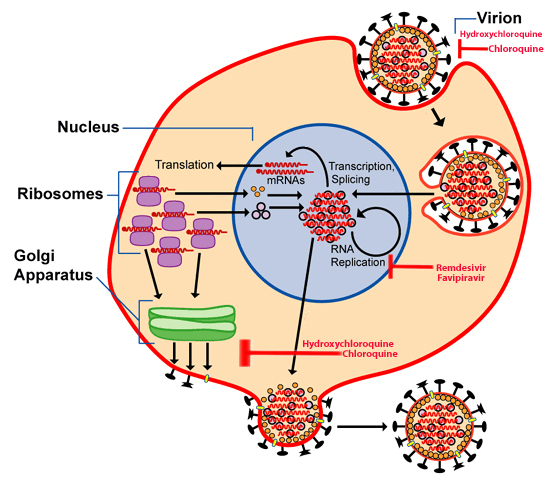
Hydroxychloroquine and chloroquine are drugs that inhibit the virus from entering or exiting an infected cell. Remdesivir and favipiravir interrupt the replication of the long nucleic acid chains viruses need to create copies. All of these therapies are experimental and should only be used under medical supervision.
The entire sequence of SARS-CoV2 genome has been determined and published. It is freely available for examination. The structure of the “spike” protein is determined using the genomic sequence of the virus. Viruses enter the cell using this protein as a kind of molecular “key”.
When this protein on the virus comes into contact with its “door” on the surface of a host cell, it is able to enter the cell and begin the process of transforming the cell into a replication system for the virus. These viral replicas exit the cell (sometimes causing damage) and go on to infect other cells. Coronaviruses, including SARS-CoV1 and SARS-CoV2, exit the cell by a process called exocytosis that does not damage the cell. The ACE-2 protein acts as a doorway which allows the SARS-CoV2 to enter human cells. This protein is found on many cells in our bodies (lungs, GI tract, heart). This is precisely the same protein that SARS-CoV1 uses to enter human cells (Wang et al., 2020).
Viruses cause potent immune responses
Entry of the virus into the cell causes its transformation into a virus replication machine. Therefore the infected cell is no longer able to carry out its normal function. Cells in blood vessels or airways are no longer able to efficiently move blood or gases (oxygen or carbon dioxide) throughout the body. These infected cells signal the immune system that they contain a foreign nucleic acid.
Infected cells also signal the immune system that they contain a foreign nucleic acid. After sending an “infected” signal to the immune system, cells attempt to stop viral replication.
Some corona viruses have an interesting mechanism that allows them to avoid detection by the host organism. Proteins remaining in the cell (but not packaged into new virus) can cause a fusion of the infected cells with surrounding cells. These fused cells are not able to carry out normal functions either. This interesting mechanism allows the virus to replicate without alerting immune cells to its presence (Maier et al., 2015).
After sending an “infected” signal to the immune system, cells attempt to stop viral replication. Infected cells and tissues sometimes undergo cell death (via a process called apoptosis) further decreasing their functions. If cells fail to die in an orderly fashion it results in tissue damage and causes cells in the immune system increase inflammation and swelling (edema).
All of these responses result in a general loss of the function of the infected cells. The tissues made up of these cells (in airway this leads to difficulty breathing or dyspnea). In certain individuals, such as the elderly and those with other diseases (cardiovascular, lung and kidney disease and those with diabetes), this inflammatory condition is more likely to spin out of control causing severe and critical COVID-19. As the inflammation continues, airway tissue and organs fill up with liquid and lose blood circulation.
In certain individuals, such as the elderly and those with other diseases an inflammatory condition spins out of control causing severe and critical disease. If lungs, heart and kidneys fail, the rest of the body (including the brain) is no longer able to carry out its normal functions.
The cells that make up the organs are incapable of excreting the waste normally generated by cells. They are also less capable of obtaining oxygen and nutrients. This causes organ failure. If lungs, heart and kidneys fail, the rest of the body (including the brain) is no longer able to carry out its normal functions. The person slips into a fatal coma and dies. This is the typical progression for a portion of severe and critical patients with COVID-19 (Huang et al., 2020).
Recommendations
We have discussed SARS-CoV2 and the development of COVID-19. This disease has become a global pandemic. Health authorities in the United States recommend the following steps to restrict the spread of SARS-CoV2 and avoid overwhelming hospitals. For asymptomatic individuals:
- Develop/maintain a healthy life-style with focus on exercising and a balanced diet
- Maintain social distancing practices in public places
- Wash your hands frequently
- Cover your mouth before sneezing or coughing
- Stay informed. You can use the links provided in the resources section of this document.
For people with cold symptoms (fever, cough, sore-throat, etc.):
- Stay at home
- Take and keep records of your temperature
- Use over the counter medications to control fever
- Call your physician or local hospital if you have a fever that is not controlled by medications or the cough causes fatigue.
If you have symptoms of pneumonia (difficulty breathing or continuous cough) or have been exposed to a person who is positive for COVID-19:
- Call your physician or hospital
- Call family or friends you have seen in the previous five days and ask them to stay at home and monitor their health.
This page has additional resources. You can also get the information in this article in a summarized form here.
Bibliography:
Benvenuto, D., Giovanetti, M., Salemi, M., Prosperi, M., De Flora, C., Junior Alcantara, L. C., … Ciccozzi, M. (2020). The global spread of 2019-nCoV: a molecular evolutionary analysis. Pathogens and Global Health, 00(00), 1–4. https://doi.org/10.1080/20477724.2020.1725339
Gorbalenya, A. E., Baker, S. C., Baric, R. S., de Groot, R. J., Drosten, C., Gulyaeva, A. A., … Ziebuhr, J. (2020). The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology, 5(4), 536–544. https://doi.org/10.1038/s41564-020-0695-z
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., … Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395(10223), 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Maier, H. J., Bickerton, E., & Britton, P. (2015). Coronaviruses: Methods and protocols. Coronaviruses: Methods and Protocols, 1282(1), 1–282. https://doi.org/10.1007/978-1-4939-2438-7
Parrish, C. R., Holmes, E. C., Morens, D. M., Park, E.-C., Burke, D. S., Calisher, C. H., … Daszak, P. (2008). Cross-Species Virus Transmission and the Emergence of New Epidemic Diseases. Microbiology and Molecular Biology Reviews, 72(3), 457–470. https://doi.org/10.1128/mmbr.00004-08
Shi, J., Wen, Z., Zhong, G., Yang, H., Wang, C., Huang, B., … Bu, Z. (2020). Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science, 7015(April), eabb7015. https://doi.org/10.1126/science.abb7015
Smith, T., Bushek, J., & Prosser, T. (2020). COVID-19 Drug Therapy Highlights : Antimicrobials with potential activity against SARS-CoV-2 : Clinical Drug Information, (Cdc), 1–21.
Wang, Q., Zhang, Y., Wu, L., Niu, S., Song, C., Zhang, Z., … Qi, J. (2020). Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell, 1–11. https://doi.org/10.1016/j.cell.2020.03.045
Steven, It makes me very happy that you’re taking the time to contribute to the opening of the communication channels between the general public and the scientific community. There’s a gap that must be filled and I believe it is the responsibility of the ones that hold the knowledge to ensure that it is clearly and widely communicated to the rest of us. I would just like to make an observation, especially because there are still many unknowns about the novel coronavirus. I believe it’s important to clearly state that the treatment options we have now may not necessarily be effective or the drugs of choice in the future. For people that are familiar with how the medical advances work, we know that what I just described may be expected, but if your goal is to reach the general public, I believe it is important to be as clear as you can on this is how science works, especially since some of your words can be taken as absolute truth by some of your readers.
Thanks, Ileana! I think it is important that readers of this article look at your comment. Everyone should understand that our knowledge of the COVID-19 pandemic is maturing. Right now medical professionals are using experimental drugs to manage patients symptoms and reduce viral load. There are currently case studies, individual reports and anecdotal evidence that suggest some of the medications discussed in the article are effective at these. All of us are still waiting on clinical trials for these (and others I didn’t mention) medications. Until we have results from the “gold-standard” clinical trials, recommendations on the use of any of these experimental medications should come strictly from medical health professionals.
The below statement is not correct.
“In my eyes rhodopsin absorbs dimmer light, which means light that has less energy.”
The energy of a photon is: E = hc/λ = hf
where λ is the wavelength, h is the Planck constant, c is the speed of light in a vacuum, and f is the frequency.
That means that the intensity is irrelevant to the energy, the wavelength (or frequency) is what matters. This principle is the foundation of the photoelectric effect which earned Einstein the Nobel Prize in physics.
Thank you for your comment, Andrew. The configuration of the protein rhodopsin is different in the the eyes of dogs when compared to humans. This configuration allows it to be stimulated by light at a higher wavelength (~506-510 nm) compared to absorption by rhodopsin in a human eye (~495 nm). Since both Planck’s constant and the speed of light in a vacuum are (indeed) constant, then the energy of a photon is inversely related to the wavelength of that photon. The photons absorbed by the dog’s eye have less energy than the photons absorbed by a human eye.
I think I see the problem is with the word “intense” in the sentence that follows the one you reference. I have amended it to “What this means in practical terms is that my eyes can pick up details in the dark. I wouldn’t call it night vision, but my eyes are better at distinguishing details in light humans may consider dim.”
Thank you again for contributing to the improving the entry!
Thanks for your blog, nice to read. Do not stop.
Thank you, Mark! We will certainly continue to produce work that shares the beauty and intricacy of biology.